Week CX: Despite federal ruling, Hochul says New Yorkers must still mask in ‘certain settings’
ALBANY COUNTY — Although a federal judge in Florida on Monday struck down the requirement to wear masks on planes, trains, buses, and other public transit, Governor Kathy Hochul on Wednesday said that New Yorkers will still be required to wear masks in “certain settings.”
This includes buses and bus stations, trains and train stations, subway and subway stations, and airports. It also includes homeless and domestic-violence shelters, correctional facilities, and state-regulated health-care and adult-care facilities and nursing homes.
Hochul said the requirements are because of the two new Omicron subvariants, which have caused a surge of infections, particularly in Central New York. Hochul spoke in Syracuse on Wednesday morning.
She said the mask requirements would be “very much in the short term.”
Hochul had lifted the mask-or-vax requirement for businesses in February, and the mask mandate for schools not in New York City was lifted on March 2.
Earlier this week, the state’s health department announced the first reported instances in the United States of significant community spread of two new subvariants of Omicron: BA.2.12 and BA.2.12.1.
The subvariants have been estimated to have a 23 percent to 27 percent growth advantage above the original BA.2 variant, which now accounts for 80.6 percent of COVID-19 infections in New York.
For the month of March, BA.2.12 and BA.2.12.1 rose to collectively comprise more than 70 percent prevalence in Central New York and more than 20 percent prevalence in the neighboring Finger Lakes region, the health department found. Data for April indicate that levels in Central New York are now above 90 percent.
According to the CDC, as of April 16, for New York and New Jersey, the original BA.2 Omicron variant makes up 45.7 percent of cases while the new subvariant BA.2.12.1 makes up 52.3 percent.
At Wednesday’s press conference, Hochul stressed that, while hospitalizations — a lagging indicator — are “trending up,” they are nowhere near the Jan. 12 peak with the initial Omicron surge of 12,000 hospitalizations.
Currently, New York State has six hospitalizations per 100,000 of population, Hochul said, adding that about half of those patients hospitalized with COVID were not admitted because of the virus but rather tested positive upon admission for other reasons.
While she termed new variants a “frightening phenomenon,” Hochul went over the “tool kit” New Yorkers should use. People experiencing symptoms should test at home for the virus, she said, and stay home if they test positive.
The state has amassed 92 million test kits, Hochul said, and 72 million are “out there” — at schools, nursing homes, senior centers, food banks, and more.
While the early warning provided by home tests is important, she said, the home tests have also created “a gap in information” since tests were formerly conducted at state or county agencies with clear reporting systems.
“We don’t have a clear picture,” said Hochul, adding that the state is working with local health departments to follow the spread.
“We’re not panicking,” said Hochul, noting there is no evidence that the new subvariants of Omicron have more severe impacts.
Hochul said people who test positive for COVID should consult with their doctors about treatment options, adding that the state has amassed over 80,000 treatments so there is no shortage.
She encouraged New Yorkers to get vaccinated and boosted, including a second booster if eligible.
Finally, Hochul said that the springtime weather, when fewer people are confined indoors, would mean “less likelihood of spread.”
Epicenter
As New York State is once again the epicenter of COVID-19 in the United States, Albany County this week has been designated by the Centers for Disease Control and Prevention as having a “medium” community level of the virus.
That’s a bump up from the “low” designation Albany County had carried since March 11.
County Executive Daniel McCoy reported on Tuesday the county’s seven-day average of new daily positive cases is now up to 119.1, and the infection rate (the percentage of positive tests) is at 9.1 percent.
This compares to 7.5 percent last week, 3.5 percent three weeks ago, and 2.6 percent four weeks ago. This metric is considered less reliable now that so many people use home tests.
Albany County continues to encourage residents to submit positive at-home COVID test results to the county website.
The more reliable metric, of cases per 100,000 of population, shows Albany County with 28.3 cases as of Tuesday as a seven-day average.
This compares to 21.1 cases per 100,000 last week; and 11.0 cases reported two weeks before that.
Statewide, Hochul said on Wednesday, New York has about 40 cases per 100,000. The highest count is in the Finger Lakes at 52.91 and the lowest count is in the Mid-Hudson region at 26.48 per 100,000 of population, as a seven-day average.
Hospitalizations, too, have climbed but not as drastically as with earlier infection increases. McCoy reported on Tuesday that 30 county residents are now hospitalized with the virus with three of them in intensive-care units.
Last week, 21 county residents were hospitalized with the virus, up from 13 two weeks ago.
Experts believe hospitalizations and deaths are less frequent now than with earlier surges because more people have antibodies — either from vaccination or previous infection — and treatments are more readily available.
Still, roughly 500 Americans are dying of COVID each day and McCoy on Tuesday reported two new COVID-related deaths in Albany County: a woman in her seventies and a man in his seventies fell victim to the virus. This brings Albany County’s COVID-19 death toll to 543.
“It saddens me to have to report two more residents who lost their lives to COVID complications,” said McCoy in the release. “As we continue to see more deaths and rising infection rates here and across the state, we’re reminded that COVID is not done with us yet.
“I continue to strongly encourage everyone to get vaccinated if they haven’t already, and to get their booster shots if they have. Albany County is making it as easy as possible to get the vaccine, with daily walk-ins available at our Health Department and delivery for those who need it.”
About a quarter of Albany County residents are still not fully vaccinated.
Mapping the virus
When the CDC started its three-tiered COVID monitoring system on Feb. 25, Albany County, like most of the nation, was colored yellow for “medium” or orange for “high” levels. On March 11, Albany County was colored green for a “low” level — no masks required — and had stayed that way until this week.
The designation is “determined by looking at hospital beds being used, hospital admissions, and the total number of new COVID-19 cases in an area,” the CDC says.
The advice from the CDC for a county, like Albany, labeled “medium” is three-fold:
— If you are at high risk for severe illness, talk to your healthcare provider about whether you need to wear a mask and take other precautions;
— Stay up to date with COVID-19 vaccines; and
— Get tested if you have symptoms.
The last two pieces of advice are given for counties labeled “low” and colored green.
Only in the counties labeled “high” and colored orange are people to wear masks indoors in public. The other advice remains the same.
Over 94 percent of the nation’s counties are now labeled as being at a low community level by the CDC. Just 0.43 percent are labeled as “high” and all of those counties are in New York State, save for Wyandotte County in Kansas.
The New York counties labeled “high” include Broome, Tioga, Wayne, Seneca, Cayuga, Onondaga, Oswego, Jefferson, Lewis, and St. Lawrence.
Nationwide, 175 counties, or 5.43 percent, are labeled “medium,” including 18 in New York State: New York, Nassau, Westchester, Orange, Albany, Rensselaer, Essex, Clinton, Fulton, Herkimer, Oneida, Madison, Cortland, Tompkins, Schuyler, Yates, Ontario, and Monroe.
Based on the CDC’s original four-tiered system for community transmission — low, moderate, substantial, high — which is defined largely by cases per 100,000 of population, most of New York, like Albany County, is “high” (colored red) as is most of New England and also most of New Jersey.
High transmission is over 100 cases per 100,000; substantial is between 50 and 99, moderate is between 10 and 49, and low is fewer than 10 cases per 100,000.
Under the four-tiered system, in New York, only far-west Chautauqua County is labeled “moderate” while four counties — Schoharie, Wyoming, Allegany, and Cattaraugus — are labeled “substantial.” The rest are labeled as having high community transmission.
Relaxing restrictions
On Monday, a federal judge in Florida struck down the requirement to wear masks on planes, trains, buses, and other public transit.
“The Court concludes that the Mask Mandate exceeds the CDC statutory authority and violates the procedures required for agency rulemaking under the APA,” wrote Judge Kathryn Kimball Mizelle in a 59-page decision, referring to the Administrative Procedure Act.
Mizelle was a Trump appointee and, as of Tuesday, the Biden administration hadn’t firmly decided if it would appeal the decision.
Meanwhile, the Centers for Disease Control and Prevention had the week before extended the mask mandate until May 3.
Some states, like New York, are still requiring masks on buses and subways.
Also this week, the CDC redefined parameters for travelers.
Most of the world — including all of North America, Europe, Russian, and Australia — is labeled “Level 3: COVID-19 High” for which the advice is: Make sure you are up to date with your COVID-19 vaccines before traveling to these destinations. If you are not up to date with your COVID-19 vaccines, avoid travel to these destinations.
China, India, and the western coast of Africa are defined as “Level 1: COVID-19 Low” for which the advice is: Make sure you are up to date with your COVID-19 vaccines before traveling to these destinations.
Currently, no countries are labeled Level 4 for which the advice is: Do not travel to these destinations.
Emergency extended
This week, both the state and federal governments renewed their public-health emergencies because of the ongoing pandemic.
Xavier Becerra, secretary of Health and Human Services, made the renewal effective April 16; the federal emergency was first declared in January 2020 and has been extended eight times.
On Friday, Hochul extended her disaster emergency declaration another 30 days until May 15.
She cited the continuing Omicron surge and said “New York continues to experience COVID-19 transmission, with the rate of new COVID-19 hospital admissions remaining at over 100 new admissions a day” and also said, “The state must pursue a coordinated approach to ensure hospital capacity statewide is able to meet regional needs.”
Hochul said, too, “The State government must support the municipalities and counties in their efforts to facilitate and administer vaccinations and tests for COVID-19, and to prevent the virus from continuing to spread at such rates.”
Mental health
Earlier this month, Thomas DiNapoli, the state’s comptroller, issued an audit showing that many school districts in New York lack sufficient staff for mental-health services.
“The upheaval caused by the COVID-19 pandemic created a crisis for many students in New York, but not enough is being done to make sure they are getting the information and support they need,” DiNapoli said in a statement, releasing the audit.
“The State Education Department should work with state and local entities to ensure resources to address the problem are available and prioritize mental health instruction and outreach among school districts so students and staff can recognize warning signs of distress and know how to get help,” he said, concluding, “I’m encouraged that the department responded positively to our recommendations.”
According to the American Psychological Association, over 80 percent of teens experienced more intense school-related stress due to COVID-19. The CDC reported that, in 2020, mental health emergency room visits rose 24 percent among 5- to 11-year-olds and 31 percent among 12- to 17-year-olds.
In December 2021, the United States Surgeon General issued a warning of an urgent mental health crisis among America’s youth.
DiNapoli’s audit shows that, among the three school districts covered by The Enterprise, rural Berne-Knox-Westerlo, with 752 students and three counselors, has the best ratio of counselors at 1:251.
However, BKW employs no social worker, the audit says, and has just one psychologist.
Voorheesville, a small suburban district, has 1,180 students and four counselors for a ratio of 1:295. The district also employs two psychologists for a ratio of 1:590, and one social worker.
Guilderland, a large suburban district with 4,841 students, has 13 counselors for a ratio of 1:372, eight social workers for a ratio of 1:605, and 11 psychologists for a ratio of 1:440 students.
Most of the state’s 686 districts outside of New York City, the audit says, entered the pandemic with mental-health teams that were far short of nationally recommended staff-to-student ratios:
— 19 school districts reported having no mental health professional staff at all;
— 653 (95 percent) did not meet the recommended ratio of one school social worker for every 250 students;
— 450 districts (66 percent) did not meet the recommended ratio of one school counselor for every 250 students; and
— 344 (50 percent) did not meet the recommended ratio of one school psychologist for every 500 students.
While state law does not require school districts to provide in-school mental health services to most students, the audit says, schools are often considered the natural and best setting for comprehensive prevention and early intervention services, and that the need for these services will likely increase as COVID-19–related and other life stresses continue to plague students.
DiNapoli’s office also audited mental-health education in schools statewide, surveying 22 districts.
New York was the first state requiring school districts to provide mental-health education. Given the urgency of the growing mental health crisis, State Education Department should ensure that school districts statewide have established a mental health curriculum and are using it, the audit says.
Currently, the department does not require districts to verify they’re meeting mandated mental health education standards, so it cannot be sure of what districts are, or are not, providing students, the audit says.
While all 22 surveyed districts were able to describe their mental-health curricula, only 19 provided supporting documentation to show they met the state’s minimum requirements. Three districts could not show evidence of providing mental health education in the midst of the ongoing crisis.
Auditors also found that the mental health curricula varied among the districts. The State Education Department, however, remained unaware of what any of these districts were, or were not, providing students in terms of mental-health education, the audit says.
With the stakes so high, the audit says, the department should act quickly to avert further crisis.
DiNapoli recommended State Education Department:
— Develop a mechanism to determine if school districts are providing mental health education as required by law; and
— Explore partnering with state and local entities to determine whether school districts should maintain certain staffing levels for mental health professionals.
In her response to the audit, Sharon Cates-Williams, deputy commissioner for the State Education Department, pointed out that “instruction designed to inform students about the importance of mental health as one of several dimensions of overall health and well-being is very different than the provision of mental health services.”
Mental-health services, she writes “are most often provided by a licensed mental health professional outside the school setting.”
As for mental-health education, Cates-Williams cites state law: “contents may be varied to meet the of particular school districts … and need not be uniform throughout the state.”
Responding to the audit’s first recommendation, she writes, “It is the responsibility of the members of the local board of education in conjunction with local school district administrators to develop and implement policies and practices that fulfill the statutory and regulatory requirements in a manner that meets the needs of the school community.”
The department, she says, “will explore the possibility of collecting an annual attestation from district administrators.”
On the audit’s second recommendation, Cates-Williams similarly responds, “ It is the responsibility of local school district officials and the local board of education to determine the staffing levels that meet the needs of the school community they serve.”
She goes on to cite a long list of entities the department confers with and states “the Board of Regents’ priorities include additional mental health supports for schools as evidenced by the Board’s budget and legislative request for additional funding to increase and improve Department capacity, as well as the capacity of districts to implement mental health supports in schools.”
Cates-Williams concludes, “To be responsive to this recommendation, the Department will continue the collaborative efforts with State and local entities and will persistently advocate for additional funds to support schools in these efforts.”
Breath test
Last Thursday, the United States Food and Drug Administration issued an emergency use authorization for the first COVID-19 diagnostic test that detects chemical compounds in breath samples.
The test can be performed by a trained operator at doctor’s offices, hospitals, and mobile testing sites, using an instrument about the size of a piece of carry-on luggage, the announcement said.
“The FDA continues to support the development of novel COVID-19 tests with the goal of advancing technologies that can help address the current pandemic and better position the U.S. for the next public health emergency,” said Jeff Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health, in a statement.
InspectIR expects to be able to produce about 100 instruments per week, which can each be used to evaluate about 160 samples per day. At this level of production, testing capacity is expected to increase by about 64,000 samples per month.
A large study of 2,409 individuals, including those with and without symptoms, validated the performance of the breath test, the FDA said. In the study, the test was shown to have 91.2 percent sensitivity (the percent of positive samples the test correctly identified) and 99.3 percent specificity (the percent of negative samples the test correctly identified).
The study also showed that, in a population with only 4.2 percent of individuals who are positive for the virus, the test had a negative predictive value of 99.6 percent, meaning that people who receive a negative test result are likely truly negative in areas of low disease prevalence. The test performed with similar sensitivity in a follow-up clinical study focused on the Omicron variant.
Boosters for young children
Pfizer and BioNTech last Thursday announced positive results for a booster vaccine for children ages 5 to 11.
Currently, booster shots have emergency authorization only for people aged 12 and older.
In the Pfizer-BioNTech study, which has not been peer reviewed, 140 children got a booster shot six months after their second vaccination. A month after getting the booster shot, the children showed a sixfold increase in antibody levels against the original version of the virus.
Laboratory tests of blood samples from a subgroup of 30 children, the announcement said, also showed 36 times the level of neutralizing antibodies against the Omicron variant compared with levels after only two doses.
The studies did not show the effectiveness against the coronavirus nor how long the antibodies would last.
Pfizer and BioNTech plan to submit a request for emergency use authorization of a booster dose for children ages 5 through 11 in the U.S. in the coming days, the announcement said.
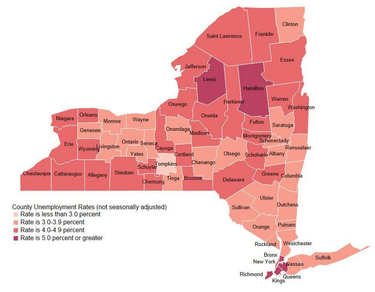
Jobs increase
On Tuesday, the state’s labor department released preliminary local area unemployment rates for March 2022 that showed a statewide decrease from 4.9 percent in February to 4.6 percent in March.
The Albany-Schenectady-Troy area had its unemployment rate fall from 8.4 percent in March 2021 to 4.8 percent in March of this year.
Albany County had an unemployment rate of 3.3 percent in March 2022.
Albany had 152,500 employed in March of this year compared to 148,000 last year, an increase of 4.5 percent.
At the same time, the number of unemployed fell from 8,500 last March to 5,200 this past March, a decrease of 3.3 percent.