Back to school in midst of pandemic
On Friday, as local schools are poised to open after Labor Day for in-person learning, the Centers for Disease Control and Prevention posted, as part of its weekly Morbidity and Mortality Weekly Report, three studies relevant to school openings.
An estimated 2 million COVID-19 cases and approximately 300 associated deaths have been reported among children aged 5 to 17 years since the start of the COVID-19 pandemic, the CDC says.
In New York State, Kathy Hochul last Tuesday, on her first day as governor, said her first priority is, “We get children back to school and protect the environment so they can learn, and everyone is safe.”
This means requiring “vaccinations for all school personnel with an option to test out weekly — at least for now,” said Hochul.
“I am also immediately directing the Department of Health to institute universal masking for anyone entering our schools,” said Hochul.
She said she would announce, later in the week, a series of school-related policies “that will be concise and consistent, giving the school districts what they have been asking for.” As of Monday, none have been forthcoming.
Local school districts have been following guidance — in the absence of requirements from the state’s health department — from the State Education Department as well as from Albany County Health Commissioner Elizabeth Whalen. Both the education department and Whalen based their advice on guidance from the American Academy of Pediatrics and from the CDC.
One of the studies posted by the CDC on Aug. 27 looked at vaccination coverage, between Dec. 14, 2020 and July 31, 2021, for adolescents between the ages of 12 and 17. Only Pfizer-BioNTech has received emergency use authorization for this age group; no vaccine has yet been approved for children younger than 12.
By the end of the study, 42 percent had had at least one shot and 32 percent had completed a vaccination series. Rates varied widely by state, ranging from 11 percent in Mississippi to 60 percent in Vermont.
“Improving adolescent COVID-19 vaccination coverage is crucial to reduce COVID-19–associated morbidity and mortality among adolescents and can help facilitate safer reopening of schools for in-person learning,” said the CDC, discussing implications of the study for public-health practice.
Although severe COVID-19 illness is more common in adults, the study says that nearly one third of adolescents aged 12 to 17 years who were hospitalized with COVID-19 from March 2020 to April 2021 required intensive care, and 5 percent of those hospitalized required endotracheal intubation and mechanical ventilation.
After the start of the COVID-19 pandemic, many schools shifted to virtual or hybrid learning. “Because in-person learning fosters social and emotional development, safely returning to schools for in-person learning remains a goal,” says the CDC.
However, given the rapid emergence and spread of the highly transmissible Delta variant and the increase in cases and hospitalizations among children and adolescents, ensuring high adolescent vaccination coverage is crucial to a safer return to the classroom, the CDC says.
“Unvaccinated or undervaccinated adolescents can become ill with COVID-19 and spread the SARS-CoV-2 virus in schools, and by extension, in local communities, placing other populations at risk,” the report goes on. “School systems can consider implementing layered prevention strategies consistent with CDC’s guidance for COVID-19 prevention in schools, including universal indoor masking regardless of vaccination status, improving ventilation, screening testing, physical distancing where feasible, and contact tracing in combination with quarantine and isolation.”
The second study posted by the CDC on Aug. 27, based in Los Angeles, looked at COVID-19 rates in prekindergarten through 12th-grade schools and the community.
Los Angeles County, the largest in the nation, has about 10 million people, including 1.7 million children and adolescents, aged 5 to 17 years.
The study, which ran from Sept. 1, 2020 to March 31, 2021, found that case rates among students were low, ranging from 110 per 100,000 in September to 859 in December 2020.
A multipronged prevention strategy, including masking, physical distancing, testing, and most recently vaccination of children and adolescents aged 12 years and older, will remain critical to reducing transmission as more students return to the classroom, the study concludes, adding, “These findings from a large and diverse county present preliminary evidence that schools provided a relatively safe environment during the 2020–21 school year.”
Notably, however, the study reflects transmission patterns before the highly contagious Delta variant became predominant in the United States.
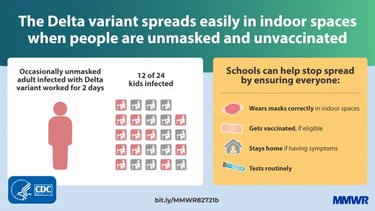
The results of the third Aug. 27 study are the most troublesome, tracing the spread of the Delta variant in a Marin County, California elementary school and community.
The Marin County teacher had COVID symptoms on May 19 but continued to teach, testing positive for the virus on May 21.
A total of 27 cases were identified. The CDC produced a chart showing where her 24 students sat (22 of them were tested); those closest to the teacher, in the front row, were all infected.
“The attack rate in the two rows seated closest to the teacher’s desk was 80% (eight of 10) and was 28% (four of 14) in the three back rows,” the study said.
“The school required teachers and students to mask while indoors; interviews with parents of infected students suggested that students’ adherence to masking and distancing guidelines in line with CDC recommendations was high in class,” the study said. “However, the teacher was reportedly unmasked on occasions when reading aloud in class.”
On May 22, students in another classroom, who differed in age by three years from the students in the class with the infected teacher and who were also ineligible for vaccination, began to experience symptoms. The two classrooms were separated by a large outdoor courtyard with lunch tables that were blocked off from use with yellow tape. All classrooms had portable high-efficiency particulate air filters and doors and windows were left open. Fourteen of 18 students in this separate grade received testing; six tests had positive results.
In addition to the documented infections in the two initial grades, cases were identified in one student each from four other grades in the school.
Transmission to community contacts, however, appeared lower than that of some previously reported Delta variant outbreak, the study said, adding, “Further transmission might have been prevented by high levels of community vaccination; at the time of this outbreak, approximately 72% of eligible persons in the city where the school is located were fully vaccinated.”
The study concluded, “The outbreak’s attack rate highlights the Delta variant’s increased transmissibility and potential for rapid spread, especially in unvaccinated populations such as schoolchildren too young for vaccination.”