COVID cases tick up this summer, new vax urged for fall
ALBANY COUNTY — Four years after the start of the pandemic here, COVID is still with us.
Governor Kathy Hochul’s Office put out a release this week to highlight an increase in hospitalizations over the same time period last year and to encourage New Yorkers to get tested if they have symptoms, to stay current with vaccines, and to seek treatment if needed.
Nationwide, the Centers for Disease Control and Prevention reports, “As of July 02, 2024, we estimate that COVID-19 infections are growing or likely growing in 39 states and territories, declining or likely declining in 0 states and territories, and are stable or uncertain in 10 states and territories.”
New York, along with neighboring New Jersey and Pennsylvania, is one of the 10 states labeled “stable or uncertain.” The others are West Virginia, New Mexico, Arizona, Washington, Oregon, Alaska, and Hawaii.
Last year, the seven-day average for COVID-related hospital admissions in New York state was 0.31 per 100,000 residents.
This year, the rate is more than double that for the same time period at 0.72 per 100,000 residents.
However, this pales compared to the hospital admissions rate for the same period in 2022: 1.66 per 100,000 residents.
Early on, health departments tracked the spread of COVID and its ever-evolving variants through required lab tests. However, as that system was dissolved, researchers at the state’s Wadsworth Lab now rely more on wastewater analysis for surveillance of circulating COVID-19 lineages.
A statewide network in New York is being used to identify fragments of the virus in wastewater. In Albany County, four treatment facilities participate. These are the latest readings, reported earlier this month:
— The North Plant sewershed serves about 109,426 people in Cohoes, Guilderland, the town of Colonie, the village of Colonie, Green Island, Watervliet, and the North End of the city of Albany.
It had a “high” reading on July 2. High detection levels correlate with more than 50 cases per 100,000 population in the past week;
— The South Plant sewershed serves about 80,922 people, covering the majority of the city of Albany.
It had a “moderate” reading on July 2. Moderate detection levels correlate with approximately 10 to 50 cases per 100,000 population in the past week;
— The Town of Bethlehem Plant serves about 31,023 people, covering the majority of the town of Bethlehem.
It had a “high” reading on July 2; and
— The Town of Guilderland Plant serves about 21,281 people, covering the majority of the town of Guilderland.
It had a “high” reading on July 3.
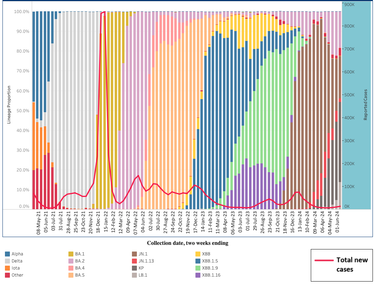
A look at the graph of new cases kept by the state’s health department shows that cases have typically dipped in the summer when people tend to be outdoors.
“As people move indoors to escape the heat, transmission does increase,” said the state’s health commissioner, James McDonald, in the release. “This is a good opportunity to remind people to improve indoor ventilation whenever possible. Additionally, the standing order I signed last year is still in effect, so anyone who would like an updated vaccine can get one at their pharmacy.”
Vaccination
Vaccinations attempt to target the latest dominant lineages of COVID-19.
The state’s health department’s graph shows the ever-changing forms of the SARS-CoV-2 virus, which causes COVID-19, beginning with Alpha, followed by Delta becoming dominant and then, at the end of 2021, the giant spike caused by Omicron.
Since then, various lineages of Omicron have flowed to dominance before ebbing.
At the end of 2023, the last vaccine targeted the XBB.1.5 variant, which was then prevalent.
The health department charts show that the dominant lineage in New York state now, at 41 percent, is KP followed by JN.1 at 22 percent, JN.1.13 at 19 percent, and LB.1 at 14 percent.
In June, the Vaccines and Related Biological Products Advisory Committee voted unanimously that the newest vaccine should target the JN.1 lineage, which followed recommendations from the World Health Organization.
“As of April 2024, nearly all (>94%) SARS-CoV-2 genetic sequences in publicly available databases are derived from JN.1, and these variants continue to displace existing XBB lineage variant,” the WHO reported.
On June 27, the Centers of Disease Control and Prevention adopted the advisory committee’s recommendations for use of 2024-25 COVID-19 vaccines, which are to be available in the fall, in people ages 6 months and older.
“It is safe to receive COVID-19 and flu vaccines at the same visit,” the CDC said in a release. “Data continue to show the importance of vaccination to protect against severe outcomes of COVID-19 and flu, including hospitalization and death.
“In 2023, more than 916,300 people were hospitalized due to COVID-19 and more than 75,500 people died from COVID-19. During the 2023-2024 flu season, more than 44,900 people are estimated to have died from flu complications.”
The CDC also said, “The virus that causes COVID-19, SARS-CoV-2, is always changing and protection from COVID-19 vaccines declines over time. Receiving an updated 2024-2025 COVID-19 vaccine can restore and enhance protection against the virus variants currently responsible for most infections and hospitalizations in the United States.
“COVID-19 vaccination also reduces the chance of suffering the effects of Long COVID, which can develop during or following acute infection and last for an extended duration.”
On June 27, the CDC’s Advisory Committee on Immunization Practices held a meeting covered by Apoorva Mandaville of The New York Times, during which data was released showing that, across every age group, a vast majority of Americans who were hospitalized for COVID did not receive one of the shots offered last fall.
Adults ages 65 and older account for two-thirds of COVID hospitalizations and 82 percent of in-hospital deaths, The Times reported, but only about 40 percent of Americans in that age group were immunized with a COVID vaccine offered last fall.
Only about 14 percent of kids under age 5 were vaccinated against COVID last fall, Mandaville reported, quoting an expert who noted that, even if children don’t have symptoms, they can bring the virus home to parents and grandparents.
“The panelists bemoaned the sharp drop in health care providers who counsel patients about the importance of Covid vaccination. Nearly half of providers said they did not recommend the shots because they believed their patients would refuse,” Mandaville reported, quoting a doctor who said, “Some of our physicians may not be recommending it due to concerns about safety of them and their staff.”
Under the Affordable Care Act, most health insurance plans currently cover the cost of COVID-19 vaccines, without the need for co-pays. People who are uninsured, or whose insurance does not cover the updated vaccine, will have access to the shots free of charge through community health centers and pharmacies participating in Health and Human Services Bridge Access Program.
However, the Bridge program is expected to end in August, just about when the new shots will become available.
Changed guidelines
Descendents of the JN.1 variant, including other variants starting with JN or KP or LP are collectively called FLiRT — all Omicron descendants. FLiRT is now causing the most cases nationwide.
The Centers for Disease Control and Prevention says there is no indication that FLiRT symptoms are any more severe than symptoms caused by earlier lineages of the virus.
Symptoms —which can include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, diarrhea — may appear two to 14 days after exposure and range from mild to severe, the CDC says.
The CDC updated its guidance on COVID-19 in March; it was the first revision in COVID-19 guidelines since 2021.
The guidelines are meant to target respiratory viruses — like the flu and RSV as well as COVID — more broadly and be easier for the public to follow.
The “core strategy” outlined by the CDC is to “stay home and away from others (including people you live with who are not sick) if you have respiratory virus symptoms that aren’t better explained by another cause.”
People can return to normal activities when, for 24 hours, symptoms are getting better and they have not had a fever.
“When you go back to your normal activities,” the CDC says, “take added precaution over the next 5 days, such as taking additional steps for cleaner air, hygiene, masks, physical distancing, and/or testing when you will be around other people indoors.”
People with symptoms should test for COVID-19, the recent release from the governor’s office said, adding, “Those who test positive should contact their health care provider about possible treatments, which have been shown to be effective at reducing the chances of serious outcomes.”
Elderly New Yorkers and those who are immunocompromised, have lung or cardiovascular conditions, or other risk factors “are especially encouraged to discuss COVID-19 treatments with a health care professional,” the office advised.