Narcan saves lives and is easy for anyone to get and use, expert says
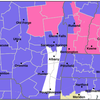
HILLTOWNS — About a month after the rural Hilltowns had two opioid overdoses on the same day, Feb. 17, Brenda Hansson will teach people about opioid addiction and life-saving naloxone-administration in a session at the Westerlo Public Library.
And she’s looking for more venues to spread the word.
In Albany County this year, just two months in, there have been a total of 25 suspected overdoses, four of which were fatal, and naloxone was used 16 times as of Feb. 28, Hansson told The Enterprise, sharing data from the Counterdrug Task Force of New York.
In 2022, there were 72 suspected overdoses in the county, 13 of which were fatal, with naloxone being administered 53 times.
Albany County Sheriff Craig Apple described the two overdoses, which happened in Rensselaerville the morning of Feb. 17 and in Westerlo later in the evening, as a reminder “that the opioid epidemic reaches all areas of our community including the often overlooked rural communities.”
Both patients were successfully treated with Narcan, a name-brand for the medication naloxone, which neutralizes the effects of opioids and can reverse an overdose.
Apple said that both patients had taken what they believed were hydrocodone pills they had obtained illicitly, which may have had some amount of fentanyl, a painkiller that is between 50 and 100 times more potent than other varieties of painkiller, including heroin and morphine.
“Many street drugs, including counterfeit prescription pills such as hydrocodone, are being laced with the deadly opiate Fentanyl which can cause life threatening side-effects,” Apple wrote in his Facebook post about the Feb. 17 overdoses. “Due to the close proximity of these overdoses, we are warning the public that there could be a deadly batch that may be being distributed throughout these small communities.”
Hansson, the opioid response program coordinator for Hudson Mohawk Area Health Education Center — the group that’s putting on the Westerlo Library event — told The Enterprise this week that illegally-manufactured drugs present a large risk for users, since their composition is less certain than in drugs made by pharmaceutical companies.
Hansson said that people can buy counterfeit prescription medications, which are designed to look like the kinds of drugs sold at a pharmacy, online through what can appear as “legitimate websites.”
Fentanyl, she said, is a common addition to these pills, and testing may also turn up rat poison, dust, and feces.
“A lot of times what happens, especially with teenagers … is somebody says, ‘Here, I got these [pills] off the internet. You want one?’ And they take one and the next thing they know, they’re overdosing,” Hansson said.
The effects of these laced drugs are all the more dangerous if they’re taken in combination with other substances, like alcohol. Because alcohol and opioids are both nervous-system depressants, they achieve a synergistic effect, Hansson said, compounding each other in ways that can be difficult to anticipate.
This can even be seen, she said, in situations that fall well within the realm of social and legal acceptability, and with substances less powerful than fentanyl.
Hansson said she’d heard of cases where EMS workers attend to someone who mixed a prescribed dose of a medication with a small amount of alcohol.
“Maybe it’s for dental surgery, or whatever, but they get a legitimate prescription for an opioid, and they take their evening pills and have a glass of wine, and the next thing you know, they’re having an overdose,” Hansson said.
“Basically,” she said, “using prescription medication with anything else without your doctor’s approval is like playing Russian roulette.”
Treating an overdose
One benefit of opioid-overdose treatment is that it can take place immediately and without the presence of medical professionals, so long as someone in proximity to an overdose victim has naloxone available and knows how to administer it.
Obtaining naloxone is easy, since anyone can get it from a pharmacy without a prescription, and it’s fairly cheap, especially with health insurance. The website GoodRx shows that the full price of naloxone at most area pharmacies is between $70 and $90. Digital coupons bring the cost down from anywhere between $30 and $70, even without insurance.
With insurance, Hansson said, the copay is often less than $40. On top of that, New York State will cover up to $40 of a naloxone copay through its Naloxone Co-Payment Assistance Program.
Administering naloxone is also easy, with Hansson saying that training takes about five minutes. Narcan provides a training video through YouTube that can be viewed at this link: bit.ly/NarcanLesson
There’s no danger associated with administration, Hansson said, since it has no effect on anyone who’s not experiencing an overdose.
Naloxone works by blocking opioid receptors in the brain, Hansson said, depriving opioids of their ability to affect the nervous system. Opioid overdoses occur when the effect on the nervous system is so strong that the respiratory system can no longer work effectively, she explained, and this process can start immediately after taking too much of a drug or as long as 90 minutes out.
“Somebody may become groggy,” Hansson said. “They may have trouble staying awake ... Normally, if somebody’s just tired, and they’re nodding off in, say, a classroom setting, when you shake them they’ll perk back up again. In an overdose situation, they’re not going to perk up. They may, for a second, open their eyes or something, but then they’ll go right back into it.”
A victim may also be making gurgling sounds, or snoring very loudly, she said, and their skin may change color to blue or gray around their lip and nail beds; with a high enough dose, “that person will essentially stop breathing.”
Hansson said that the first thing to do when in the presence of someone experiencing an overdose is to try and wake them and, if possible, perform CPR.
One technique Hansson’s group teaches is “something called a sternum rub,” she said, “where basically you make a fist and take your middle knuckle and grind it into their breastbone. That will wake you up if you’re just asleep.”
After that, it’s important to call 9-1-1, Hansson said, and, once emergency services are on the way, the person can begin administering naloxone.
“Somebody who has an active addiction always has the chance to turn their lives around,” Hansson said. “They can stop using drugs and have a productive life. If they die, they obviously don’t get that chance. Giving somebody Narcan is basically just giving them a second chance to really kind of look at what they’re doing to themselves and seek help.”
Fighting stigma
A major aspect of Hansson’s work is combating the stigma that exists around drug use and overdoses, which can be counterproductive by getting in the way of investment in treatments, or tolerance for people who suffer from it. It’s something that she said she’ll address at the Westerlo event.
“I certainly don’t want to be preachy to people who come out for Narcan training,” she said, “but I do want to bring out a little bit of information about how people tend to look at people who are drug users in our society without really realizing that a lot of people who end up with opioid problems start with a prescription from their doctor — a legitimate prescription for legitimate pain … It’s often not a stereotypical drug-user scenario,” she said.
People can also be surprised at how quickly and powerfully addiction sets in, she said, especially when they themselves don’t have an addictive predisposition or experience with someone who does.
Treatment for addiction can be hard to come by in rural settings like the Hilltowns, since services are often located far away, and people may resist placing services within their own communities because of their negative view of addiction and drug-users.
The Enterprise reported in 2021 that the Berne Town Board at the time was unreceptive to the county’s interest in establishing a drug and mental-health counseling office in the town’s senior center, due to negative feelings held by some of the town’s seniors. The proposal did not move forward.
“I can tell you the term ‘violently opposed’ is not unreasonable here,” then-Councilman Mat Harris said of the senior population’s attitude toward the proposal at the time.
Karen Stark, a senior who coordinated the county’s senior meals program, which brings seniors into the Berne senior center three days a week for approximately three hours each day, told The Enterprise then that she had concerns about seniors’ safety.
“It’s more or less that the people coming in [to the center] are mental or on drugs, and my seniors are in there …,” Stark said, “I don’t want our seniors to be at any risk at all.”
Hansson said she’s hoping to hold more informational and training events locally, and has reached out to other organizations but has yet to solidify anything.
“It’s a learning process with everybody,” she said. “Stigma and harm reduction are our [organization’s] two biggest pieces, and we just have to keep chipping away, helping people to shift their perspective on it.”
****
The Hudson Mohawk Area Health Education Center will host a free informational training session, open to the public, on March 21 from 6:30 to 8:30 p.m. at the Westerlo Public Library, located at 604 NY-143, Westerlo, New York 12193.