Capital Region does well getting the vaccine it has into arms
ALBANY COUNTY — Although the clamor continues for COVID-19 vaccinations as demand far outstrips supply, the Capital Region is doing well getting the vaccine it has into the arms of residents, according to figures released by the governor on Friday.
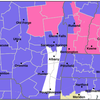
The Capital Region has administered 92 percent of first and second doses of the vaccine it has received. Of the state’s 10 regions, only two others have a higher rate: the North Country at 94 percent and the Southern Tier at 93 percent. New York City has the worst rate, at 63 percent.
The numbers are based on the first four weeks of availability for non-long-term care facilities. Vaccine is distributed to each region based on population.
“We have the demand … We just need the supply,” said Albany County Executive Daniel McCoy at his Friday morning press briefing.
He urged patience and noted residents who “aren’t computer savvy” can call 2-1-1 to get help navigating the state’s Am I Eligible website to sign up for shots. Over 240 people called the first day.
“If you got in for your first shot, you do not have to register for a second shot,” he stressed.
McCoy noted that county offices had been reaching out to residents aged 75 and over and “a lot of them said no.”
He praised Bill Clay, the chairman of the Albany County Legislative Black Caucus, for getting pictured as he got the vaccine. “He believes in the vaccine — it’s safe,” said McCoy.
With the latest federal guidance, about 7 million New Yorkers are eligible to be vaccinated yet the state had been receiving just 300,000 doses each week. That supply is expected to dwindle to 250,000 Governor Andrew Cuomo said in his press briefing on Friday.
“Of the new allocation, the faster sites will get more of the new allocation. Why? Because they get it out the door faster, and this is about getting needles in arms,” said Cuomo. “No one gets all they need.”
He was critical of the federal decision last week to add people 65 and older to the category of eligible vaccine recipients.
“What they did was like opening the floodgates of eligibility and you have a rush of 7 million people, ‘I want a vaccine. I want it now. I was told I’m eligible.’ And that entire flood has to go through a syringe,” said Cuomo. “All this volume and it has to go through the point of a needle literally and figuratively, that’s the situation that the federal government created.”
A month ago, the plan was to vaccinate frontline health-care workers first, in tier 1a, followed by essential workers and people 75 and older, in tier 1b. Adding people 65 and over added 1.8 million New Yorkes.
“There are only 15 million New Yorkers eligible to begin with, because the vaccine is 16-plus, right?” said Cuomo, referencing the fact that youth are not to get vaccinated. “So, roughly half the population is now eligible.”
New York State started with naming a hospital to be a hub for each of the state’s 10 regions. Albany Medical Center is the hub for the Capital District, which serves eight counties including Albany.
Cuomo is continuing to push to get hospital workers vaccinated, both to keep hospital beds available and to prevent spread of the virus.
Albany Med, Saratoga Hospital, Glens Falls Hospital, Ellis Hospital, and St. Peter’s Hospital — all in the Capital Region — are among the health-care centers that have distributed 100 percent of allocated vaccine doses, meaning they administered all first-dose vaccines they have been given.
Approximately 81 percent of Albany Med’s and 85 percent of Glens Falls Hospital’s health-care workers have received the vaccine; according to a release from Albany Medical Center; the percentage of hospital workers who declined a vaccine in the Capital Region is 11.7 percent — the lowest rate in New York State.
On Friday, Cuomo outlined the expanding network for administering vaccinations. “We have about 5,000 pharmacies; about 194 hospitals; you have about 2,500 private doctor networks; city departments of health, county departments of health: 58, and then we have state mass vaccination sites, which were just very high-volume vaccination sites,” said Cuomo.
Five mass-vaccination sites — including one at the University at Albany, which opened on Friday — are up and running. Fifteen more are planned across the state.
Also on Friday, the state launched a program to bring vaccination sites into places without doctor’s offices or pharmacies. “A health-care desert is a health-care desert because it doesn’t have traditional distribution. So we’re supplementing that …,” said Cuomo. “That’s public housing, churches, and community centers. We're setting up mass vaccination sites.”
Cuomo said that city and county health departments are to prioritize police, firefighters, and public-safety workers while hospitals prioritize nurses and doctors, and pharmacies and private practices focus on people 65 and older.
The state is still waiting for clear guidance and which categories of people are now eligible, under the federal expansion, for underlying health conditions, Cuomo said.
“The current federal government — which is going to be current for a couple of days, right? — they recommend adding, now, people with pre-existing conditions,” Cuomo said. “We have seven million currently eligible. That would add about 5 million people. You would then be at 12 million people, we only have 15 million people statewide.”
The governor did share some good news: “Ninety-six percent of nursing home residents have gotten the vaccine, and it's going to be complete by Sunday,” Cuomo said.
But he also said that another case of the highly transmissible B.1.1.7 variant of COVID-19 has been confirmed in New York State, in Nassau County, bringing the state’s known total to 16.
Cuomo stressed, “Hospital capacity is still the red line, danger zone, shut-down mechanism in this entire situation. California is what we're afraid of. Italy is what we're afraid of. UK is what we're afraid of … If the hospitals are overwhelmed, you close down. Period. End of story. You close down, everyone closes down. Every restaurant. Every office. We go right back to full shutdown.”
He noted that hospital capacity depends both on the number of available beds and the staff to attend to the patients in those beds.
“Unfortunately, we’ve had 29 hospitalization overnight, which is the most we’ve had in one night,” McCoy said at his Friday morning press briefing.
Currently 168 county residents are hospitalized with COVID-19, which McCoy termed “a record we did not want.” The former record was set on Jan. 7 with 163 residents hospitalized with the virus.
The death count follows hospitalization. Three more county residents died of COVID-19 on Thursday — a woman in her fifties, a woman in her eighties, and a woman in her nineties.
Sixty-three county residents died of COVID-19 in December, a record McCoy says he does not want to break. So far in January, 39 residents have died of the disease.
County POD
“We’re not getting the number of vaccines that we want yet and we are able to give more,” said Albany County Health Commissioner Elizabeth Whalen.
Her department applied for a larger allotment last week and received 500 doses. “I’m happy to say we went through everything we received,” said Whalen.
A point of dispensing, or POD, was set up Thursday at the Times Union Center in Albany, which could accommodate people in wheelchairs or who had trouble walking. The process, which began with screening questions and ended with a waiting period to be sure there were no negative reactions, took the average person eight to 15 minutes, Whalen said.
People who in the past had suffered severe allergic reactions waited for 30 minutes. “We have not had anyone experience ill effects,”said Whalen.
She noted there has been “a lot of confusion” with links, some of them to bogus clinics or test clinics and advised using only two websites: the state’s Am I Eligible site, and the CapitalRegionVax site run by Albany Medical Center.
Like the governor, Whalen said that hospitals need to focus on vaccinating frontline health-care workers.
Of the county’s upcoming vaccine supply, Whalen said, “We don’t really know what next week will bring. We are hopeful that we will get the amount we requested …. It’s the supply that’s the rate-limiting step.”
She said of her department, “We don’t schedule until we know what we’re going to get.”
Whalen also said “I ask for patience and I ask for continued vigilance.”
She stressed the importance of wearing a mask even after getting vaccinated. It takes a couple of weeks after getting the second dose for antibodies to form, she said.
Newest numbers
As of Friday morning, Albany County has had 15,284 confirmed cases of COVID-19, including 292 new cases since Thursday, McCoy announced.
Of the new cases, 236 did not have a clear source of infection identified, 43 had close contact with someone infected with the disease, and 13 are health-care workers or residents of congregate settings.
The five-day average for new daily positives has increased to 269.8 from 267.2. There are now 2,035 active cases in the county, up from 1,981 yesterday.
The number of county residents under quarantine decreased to 3,214 from 3,438. So far, 45,442 residents have completed quarantine. Of those, 13,249 had tested positive and recovered. That is an increase of 209 recoveries since yesterday.
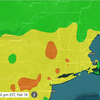
The Capital Region continues to have one of the worst rates for available hospital beds, at 25 percent. Only the Mohawk Valley is lower, at 24 percent.
Currently, 525 Capital Region residents are hospitalized with COVID-19, which is 0.05 percent of the region’s population.
Statewide, 0.05 percent of New Yorkers are hospitalized with the virus, leaving 32 percent of hospital beds available.
The Capital Region, at 20 percent, and the Mohawk Valley, at 19 percent, have the worst rate for available intensive-care-unit beds. Currently 210 of the Capital Regions’ 254 ICUbeds are filled.
Statewide, 27 percent of ICU beds are available.
The Capital Region’s infection rate, as a seven-day average, is at 7.94 percent. Two areas — the Mohawk Valley and Long Island — have a worse rate. Statewide, the positivity rate is 6.67 percent.
“There’s still personal responsibility and it’s still purely a function of how a community acts,” said Cuyomo about high rates of infection.