Week XCV: As Omicron spikes, state sets up two new testing sites in county
The Enterprise — Michael Koff
“We know that tests are right now a scarcity. If you are feeling … unwell, you should obtain a test if you can but for now … given the spread we are seeing, I would assume your symptoms are attributable to COVID-19,” said Albany County Health Commissioner Elizabeth Whalen on Friday.
ALBANY COUNTY — Albany County, in its 95th week of coping with coronavirus, was gripped, like the rest of the state and nation, in an unprecedented surge of new COVID-19 cases spurred by the highly transmissible but thought-to-be milder Omicron variant.
Albany County Executive Daniel McCoy held a press conference on Friday, announcing 1,003 new cases in a single day, nearly tripling the county’s former high last Jan. 12 of 351 cases — before the vaccine was widely available.
The daily numbers since then have been in the 200 to 400 range but soared to 733 new cases on Tuesday. McCoy surmised they are artificially low numbers since tests have been hard to come by and also because people who have located scarce at-home antigen tests may not have reported results.
The county has set up an online system, asking residents to fill out a form if they have tested positive for COVID-19: Go to www.AlbanyCounty.com and follow the red COVID-19 information bar at the top of the page to report positive results.
So far, county spokeswoman Mary Rozak said on Monday morning, 800 positive tests had been reported through the portal, which was set up last Thursday. “It continues to grow,” she said.
At the same time, the state has announced two testing sites in Albany County. One, at Crossgates Mall in Guilderland, at the former site of Ruby Tuesday restaurant, opened on Tuesday. Appointments can be booked at https://www.gogettested.com/.
The other, at the uptown University at Albany campus, will be held in the Colonial Dining Hall at 1400 Washington Ave. Beginning Jan. 7, the hours of operation are 8:30 a.m. to 4 p.m. Appointments may be scheduled here.
The Crossgates site administers antigen tests while the UAlbany site will administer polymerase chain reaction tests.
PCR tests are sent to a lab to screen for the presence of viral RNA, which is detectable in the body before antibodies form or symptoms of the disease are present; PCR tests may also come back positive after symptoms have faded. Antigen tests, which show results in 15 minutes without a lab, are best at identifying COVID-19 when symptoms are present.
McCoy said on Friday that the county’s health department would not be able to call everyone to quarantine or isolate. “It’s physically impossible to keep up with everything,” he said.
However, on Monday, Rozak told The Enterprise that those calls will be made — it’s just a matter of time.
“We are still doing contact tracing ... It’s the sheer volume that’s buried us. It’s not like we put our hands up and said, ‘We’re not doing this anymore.’ That’s not the case at all,” said Rozak.
The way the state set up the databases is problematic, Rozak said. “All that we essentially get, when we find out about positives, is a name, a date of birth, and a phone number.”
So, she said, there is no way to quickly sift through to find out who may be at high risk to call them first.
The state has told the county’s health commissioner, Elizabeth Whalen, that it may set up a portal to make it easier “but who knows if it will happen fast enough,” said Rozak.
Right now the county is going through the cases as they come in, she said, creating a “heavy, heavy workload” so it’s taking longer to get to people.
Residents who test positive are encouraged not to wait for a call from the health department to start isolating; rather, they should go to the county’s website to follow the guidance for isolating. Similarly, those who have been exposed to the virus can consult the website for quarantine protocols.
Currently the calls to those who test positive are being handled by county health department workers and staff from other county departments who are experienced with the process.
Hospitalizations
This week, hospitalizations also increased to new levels in Albany County.
McCoy reported on Tuesday that 99 county residents are now hospitalized with the virus — 11 of them are in intensive-care units. He also said that seven of the hospitalized residents were younger than 25 years old.
On Wednesday, he reported 25 new hospitalizations with a total of 109 county residents currently hospitalized with the coronavirus — a net increase of ten. Twelve of those hospital patients are in intensive-care units.
“The number of county residents in the hospital has now more than doubled from the 51 individuals we reported the day after Christmas, further straining our hospital system that has already been impacted by healthcare workers getting infected after the latest surge of COVID cases,” said McCoy in his Wednesday morning COVID release.
While Omicron has so far — based on studies in South Africa and Britain where it peaked first — proved to be milder than the Delta variant, just the sheer number of infections could still strain the hospital system.
“We get the cases, then two weeks later, we get the hospitalizations, and then a couple of weeks later, we get the deaths,” said Whalen on Friday.
“We know what we don’t want to happen,” she said, stressing the importance of protecting hospitals from being overwhelmed. “We’re just starting to see the beginning of the spike right now,” she said.
The state’s health department has found that the number of laboratory-confirmed break-through cases — in which fully vaccinated New Yorkers developed COVID infections — through Dec. 28 amounts to 3.4 percent of those 12 and older who were vaccinated and .12 percent of those who were hospitalized.
The health department also reports that the vaccines, which were 92.3 percent effective in May plateaued to 80 percent effectiveness in July after the Delta variant became predominant, and now most recently with the Omicron variant are about 75 percent effective.
Fully-vaccinated New Yorkers had between a 90.2 percent and 95.7 percent lower chance of being hospitalized with COVID-19, compared to unvaccinated New Yorkers, the health department analysis concluded.
“We’re being overrun right now in our emergency departments with patients coming in with very mild symptoms, or some with no symptoms, requesting COVID testing,” said St. Peter’s Health Partners Chief Medical Director of Acute Care Thea Dalfino at the Friday press conference. “So we’re making a plea to the community.”
The plea is to use at-home tests — “if you can find them,” said Dalfino — or go to a primary-care provider or urgent-care center for tests. Those venues are also seeing long lines locally.
“Our emergency departments really are for the sickest patients,” Dalfino said.
She also said, “We’re encouraging those who have mild symptoms, you may not even need to go get tested. We want to be able to have our testing supplies for those who are sickest and that we could potentially treat.”
Whalen said on Friday, “We know that tests are right now a scarcity. If you are feeling … unwell, you should obtain a test if you can but for now … given the spread we are seeing, I would assume your symptoms are attributable to COVID-19.”
Whalen also said, “We are starting to see what we had forecasted, which is exponential spread. This is likely due to the Omicron variant.”
Data from sequencing at Wadsworth Laboratory, which does about 100 per day from across the state, showed a marked increase of the Omicron variant in December. From Dec. 5 to 18, Whalen said, Omicron accounted for 30.9 percent of the positive tests; from Dec. 15 to 28, Omicron accounted for 74 percent.
On Tuesday, the CDC estimated that nationwide, 92 to 97 percent of the new COVID-19 cases in the period between Dec. 25 and Jan. 1 were the Omicron variant. The estimate for the New York State and New Jersey area was 98 percent.
The governor’s office on Tuesday reported that the Omicron variant comprised 93.8 percent of uploaded sequences from New York State between Dec. 21 and Jan. 3. This is based on data from the Global Initiative on Sharing Avian Influenza Data and has fluctuated in the 90s throughout the week.
“The forecast, with modeling that’s being done, is this will peak quickly,” said Whalen. If the Omicron variant in New York State performs as it did in South Africa and the United Kingdom, said Whalen, numbers will likely continue to grow until probably the end of January and then, she said, “we will hopefully see a steep drop-off.”
Whalen stressed, “This is a critical time.” She went over the protocols she has been encouraging for months — mask-wearing, social-distancing, hand-washing. “The work you’re doing now may save a life,” said Whalen.
Waiting for state guidance
People may be confused, Rozak told The Enterprise on Monday, because of guidance sent out by the state’s health department on essential workers who have tested positive returning to work after five days instead of 10.
Rozak shared the Dec. 24 guidance with The Enterprise, which states, in part: “In limited circumstances where there is a critical staffing shortage, employers may allow a person to return to work after day 5 of their isolation period” is they are fully vaccinated, asymptomatic, haven’t had a fever for 72 hours, and can wear a well-fitting mask like a KN95.
The guidance includes a list of essential workers.
A company has to determine who is an essential worker, said Rozak, positing that a worker could become essential because of staff shortages. “Some of it is up to the judgement of employers,” she said, noting she has fielded many questions about that.
On Dec. 27, the Centers for Disease Control and Prevention issued new guidance on isolation and quarantine periods.
“Given what we currently know about COVID-19 and the Omicron variant, CDC is shortening the recommended time for isolation from 10 days for people with COVID-19 to 5 days, if asymptomatic, followed by 5 days of wearing a mask when around others,” says the new guidance.
Most transmission occurs early in the course of illness, generally in the day or two prior to onset of symptoms and then two to three days after, the CDC says.
The CDC also changed the quarantine period for people exposed to COVID-19.
People who are vaccinated and have a booster shot — six months after the second shot of Moderna, now five months after the second Pfizer-BioNTech shot, and two months after the single-shot Johnson & Johnson — do not need to quarantine after being exposed, but should wear a mask for 10 days after the exposure.
For people who are unvaccinated or are more than five or six months out from their second messenger RNA dose or more than two months after the J&J vaccine and not yet boosted, the CDC now recommends quarantine for five days days followed by strict mask use for an additional five days.
“Alternatively, if a 5-day quarantine is not feasible, it is imperative that an exposed person wear a well-fitting mask at all times when around others for 10 days after exposure,” the guidance says.
Anyone who has been exposed to the virus should get a COVID test the fifth day after exposure, the CDC says. If symptoms occur, the exposed person should immediately quarantine until a negative test confirms symptoms are not attributable to COVID-19.
The 10-day period has not changed statewide, including for schools, because New York has not issued new guidelines. “We follow the state guidelines,” said Rozak of Albany County.
“Dr. Whalen believes there will be an update from New York State this week. She will then update the school districts,” said Rozak.
Schools
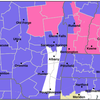
Schools reopened for in-person instruction on Jan. 3 after winter break. Governor Kathy Hochul’s plan is for students who may have been exposed to COVID-19 to take home rapid antigen tests; if the test is negative and the student is asymptomatic, he or she can return to school rather than quarantining.
Locally, the Capital Region Board of Cooperative Educational Services is distributing the rapid antigen tests. “Please note that any positive test results from an at-home test must be reported to the local health department and to your school nurse,” said local school notices this week, including at Guilderland and Berne-Knox-Westerlo, both in the Capital Region BOCES.
Rozak was emphatic on Monday, saying that the only way anyone should inform the county health department of a positive test result is through the county’s website, which has a link for that purpose.
“No calling,” she said. “Because right now they’re making all the calls outbound. It’s just impossible for someone to call in.”
Also important, she said, is: “You have to have a picture of the rapid-antigen test because that’s critical.”
Local schools, like those across the state, reported a jump in COVID-19 cases after a 10-day winter break.
According to the state’s tracker, as of Jan. 4, Guilderland, with about 4,800 students, had 467 cases this school year, a jump of 174 over the pre-vacation Dec. 23 number of 293 confirmed cases. Student cases remained the vast majority with 379 cases reported — a jump of 132.
Voorheesville, with about 1,200 students, has had 136 confirmed cases — a jump of 56 from Dec. 23 with student cases increasing by 44 from 69 pre-vacation to 113 on Jan. 4.
Berne-Knox-Westerlo, with about 780 students, has had 133 confirmed cases — an increase of 24 from Dec. 23 with student cases increasing by 18 from the pre-vacation number of 78 to 96 on Jan. 4.
Surge ongoing
At a press conference in Plattsburgh last Wednesday, Hochul noted the uptick in cases statewide and said, “So we’re basically preparing for a January surge. We know it’s coming and we’re naive to think it won’t.”
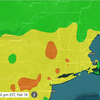
On Tuesday, the governor’s office reported the statewide infection rate, as a seven-day average, at 21.81 percent. The highest rate is on Long Island at 25.49 percent and the lowest is the North Country at 13.37 percent. Albany County, according to the state’s dashboard, had a 21.4 percent positivity rate.
Johns Hopkins, which has been tracking positivity rates across the United States since the spring of 2020, reported on Tuesday that just one state, Wyoming, with a rate of 4.37 percent, is below the 5-percent threshold set by the World Health Organization.
On May 12, 2020, the WHO advised governments that, before reopening, rates of positivity in testing — that is, out of all tests conducted, how many came back positive for COVID-19 — should remain at 5 percent or lower for at least 14 days.
Johns Hopkins reports New York State’s seven-day average at 14.61 percent. The state with the highest rate is New Jersey at 86.75 percent.
“If a positivity rate is too high, that may indicate that the state is only testing the sickest patients who seek medical attention, and is not casting a wide enough net to know how much of the virus is spreading within its communities,” says the Johns Hopkins site.
“A low rate of positivity in testing data can be seen as a sign that a state has sufficient testing capacity for the size of their outbreak and is testing enough of its population to make informed decisions about reopening,” says Johns Hopkins.
Again, since residents are under no obligation to report results of at-home tests, numbers, as McCoy noted, may be artificially low.
Also on Tuesday, the governor’s office reported, as a seven-day average of COVID cases per 100,000 of population, New York State was at 344.18. Albany County, according to the state’s dashboard, was at 155.8.
FDA update
On Monday, the United States Food and Drug Administration amended the emergency use authorization for the Pfizer-BioNTech COVID-19 vaccine to expand its use in three ways.
People aged 12 to 15 years old can now get a Pfizer booster shot.
The time between a second Pfizer shot and a booster shot has been reduced from six months to five months for people who are 12 and older.
And a third primary series dose is now authorized for certain immunocompromised children 5 through 11 years of age. Children in this age group who have undergone solid organ transplantation, or who have been diagnosed with conditions that are considered to have an equivalent level of immunocompromise, may not respond adequately to the two-dose primary vaccination series, the FDA says.
Children 5 through 11 years of age who are fully vaccinated and are not immunocompromised do not need a third dose at this time, the FDA says, but it will continue to review information and communicate with the public if data emerges suggesting booster doses are needed for this pediatric population.
“Throughout the pandemic, as the virus that causes COVID-19 has continuously evolved, the need for the FDA to quickly adapt has meant using the best available science to make informed decisions with the health and safety of the American public in mind,” said Acting FDA Commissioner Janet Woodcock, in a statement.
“Based on the FDA’s assessment of currently available data, a booster dose of the currently authorized vaccines may help provide better protection against both the delta and omicron variants,” said Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, in a statement. “In particular, the omicron variant appears to be more resistant to the antibody levels produced in response to the primary series doses from the current vaccine.
“With this in mind, the FDA has extended the range of individuals eligible to receive a booster, shortened the length of time between the completion of the Pfizer primary series for individuals to receive a booster and is authorizing a third protective vaccine dose for some of our youngest and most vulnerable individuals.”
Support for childcare
The Capital Region has received $31,222,838 in federal funds to support childcare.
The state has awarded $900 million in Child Care Stabilization Grants to programs across New York, Hochul announced on Thursday. The grants are part of a $2.3 billion package funded by the federal American Rescue Plan Act and Coronavirus Response and Relief Supplemental Appropriations Act.
The Office of Children and Family Services awarded funding to nearly 15,000 eligible child-care providers over four months, from August through November.
The office is administering the funds to cover the costs of personnel, rent or mortgage, utilities, facility maintenance or improvements, personal protective equipment, supplies needed to respond to COVID-19, goods and services needed to maintain or resume child-care services, mental health supports for children and employees, and health and safety training for staff.
Newest numbers
Three more Albany County residents died of COVID-19 this week, bringing the county’s death toll from the virus to 473. On Monday, a man in his fifties and a woman in her sixties succumbed to the virus and on Tuesday a woman in her eighties died, McCoy reported.
With the 733 new COVID-19 cases, Albany County on Wednesday had 3,949 active cases, up from 3,500 on Tuesday. The number of county residents under quarantine increased to 4,535 from 4,072.
As of Tuesday, 79.1 percent of all Albany County residents have received at least the first dose of the vaccine, and 71.8 percent have been fully vaccinated. The first-dose vaccination rate for county residents 18 and older is 88.0 percent.
According to the state’s vaccine tracker, 84 percent of New Yorkers have received at least one dose of vaccine as have 95 percent of New Yorkers 18 and older while 71.8 percent of New Yorkers are fully vaccinated as are 82.9 percent of New Yorkers 18 and older.