Community Caregivers, a not-for-profit organization dedicated to enabling individuals of all ages to maintain their independence, dignity, and quality of life within their homes and communities, has announced its 24th annual gala raised $68,000.
Held Nov. 17 at Albany Country Club in Voorheesville, the gala was attended by more than 165 people.
The evening featured silent and live auctions and a wine-and-dine pull. Greg Floyd, news anchor at CBS 6 Albany, served as this year’s master of ceremonies. The board of directors wishes to thank gala sponsors Adirondack Environmental Services, Albany Med, Ayco Charitable Foundation, Bank of America, MVP Health Care, Dr. Judith Mysliborski, New York Business Development Corporation, and United Group of Companies.
At the gala, Congressman Paul Tonko, a Democrat representing the Capital Region, presented a proclamation to Community Caregivers Advisory Board member Ellen Howie. She and her husband, Dick, have volunteered with the organization since 1995. The couple also recently celebrated their 60th wedding anniversary.
During the event, the board presented the Joseph A. Bosco Community Service award to the Capital Financial Planning Charitable Foundation. The Foundation was started in 2009 by Todd Slingerland, president and chief financial officer of Capital Financial Planning, a registered advisory investment firm located in Guilderland.
The foundation has helped to bolster the many efforts of not-for-profit organizations, including those dedicated to fighting disease and hunger, enhancing education and youth development, supporting veterans and the elderly, and working to address problems such as domestic violence and homelessness.
Each year, the foundation raises funds through its golf outing and selects a primary beneficiary to receive donations and grants. In 2018, the foundation selected Community Caregivers.
Editor’s note: Jayson White is a Community Caregivers board member and chairs its public relations committee.
Location:
November is Family Caregivers’ Month. As we celebrate Thanksgiving and usher in a season of holidays from now to the new year, it’s important to recognize that this can be a tough time of year for family caregivers. We encourage families to draw upon community resources, like Community Caregivers, and to adjust family traditions to keep the holidays joyful and meaningful.
Former First Lady Rosalynn Carter, who has been a lifelong champion for family caregivers, stated: “There are only four kinds of people in the world — those who have been caregivers, those who are caregivers, those who will be caregivers, and those who will need caregivers.”
Even though caregiving is a universal experience, we feel so alone. Families often try to cope without a lot of support.
And, primary caregivers often deny the need for help, thinking, “If I were just a better spouse (or daughter, or son), I could do this without ‘outside’ help.” However, caregiving is a marathon, not a sprint, so family caregivers need to pace themselves and guard their own mental and physical health.
And, believe it or not, for the person receiving care, socializing with someone outside the family can be refreshing and renew their interest in life.
In our local area, Community Caregivers has been supporting individuals, families, and caregivers for over two decades. Our caring volunteers offer respectful assistance.
Volunteers offer rides for those who do not drive; it’s a one-on-one service in a volunteer’s own car. Many of our volunteers seek to connect with the older residents of the community, so they offer friendly visits and regular phone calls. And our volunteers do those practical things like grocery-store runs that make living at home possible.
Community Caregivers staff do the “matching” of older adults to volunteer services. Please call us; there is no obligation simply to check out what Community Caregivers offers. In fact, thanks to our volunteers, our services are offered without a charge.
Our holidays are also bolstered by family traditions and high expectations for the perfect time as epitomized in the Hallmark commercials. Yet as families change, traditions demand that we adapt.
I see this in my own family. Each Thanksgiving, I look forward to my mother’s apple pie at our holiday table. For the past several years, however, the pies would not be baked without my sister’s assistance. It’s still Mom’s apple pie and we honor whatever contribution she makes to their creation, even though she can no longer stand at a kitchen counter or take hot food from an oven.
Family members who assist our elders know about creating new routines and altering old ones to help their loved one live life to the fullest each day. This holiday season, it’s incumbent upon those family members who live at a distance and may not have seen Mom or Dad in months to understand that the local caregiving family member is doing his or her best.
No doubt it’s a long ways from perfect. It’s common that Mom or Dad reject assistance that clearly is needed. It’s difficult to graciously accept the help of others after a lifetime of independence.
So, for those of us gathering this holiday season, it’s vital to stay flexible, communicate with compassion, and — above all — keep a sense of humor. This year, as we savor a slice of Mom’s apple pie, we will enjoy each other’s company and our new family traditions that make the holidays work for everyone.
Happy Thanksgiving from Community Caregivers to you and your family.
Editor’s note: Linda Miller is the Outreach and Education coordinator for community Caregivers.
Location:
Community Caregivers, a not-for-profit organization dedicated to enabling individuals of all ages to maintain their independence, dignity and quality of life within their homes and communities, will hold its 24th annual gala on Saturday, Nov. 17 at Albany Country Club at 300 Wormer Road in Voorheesville. This year’s gala theme is Helping Hands, Caring Hearts.
The evening will begin with cocktails at 6 p.m., with dinner and silent and live auctions at 7 p.m. The gala’s popular wine-and-dine pull will also be featured. Greg Floyd, news anchor for CBS 6 Albany, will again serve as this year’s master of ceremonies. The board of directors thanks gala sponsors Adirondack Environmental Services, Albany Med, Ayco Charitable Foundation, and Bank of America.
The board is pleased to announce the Joseph A. Bosco Community Service award will be presented to the Capital Financial Planning Charitable Foundation. The foundation was started in 2009 by Todd Slingerland, president and chief executive officer of Capital Financial Planning, a registered advisory investment firm located in Guilderland.
The Foundation has helped to bolster the many efforts of not-for-profit organizations, including those dedicated to fighting disease and hunger, enhancing education and youth development, supporting veterans and the elderly, and working to address problems such as domestic violence and homelessness.
Through its annual golf tournament held the third Monday in May at Albany Country Club, the foundation raises funds for donations and grants, selecting a primary beneficiary each year. In 2018, the foundation selected Community Caregivers. Past primary beneficiaries have included Ronald McDonald House (through the Amazing Gracie’s Gift Foundation), YMCA Circle of Champs, STRIDE Adaptive Sports, Sunnyview Rehabilitation Hospital, Ellis Medicine/Bellevue Women’s Heart Health Center, and Brave Will Foundation.
Ellen Kaufman, gala committee chairwoman, and her committee invite the community to attend and pay tribute to the Joseph Bosco awardee. Tickets are $125 per person. For ticket information, please call 518-456-2898. And to learn more about Community Caregivers, visit www.communitycaregivers.org.
Editor’s note: Regina Dubois is a Community Caregivers’ board member.
Location:
This week — Sept. 22 to Sept. 28 — marks National Falls Prevention Week. It corresponds with the start of the fall season.
At Community Caregivers, our mission is to help people stay independent as they age. Staying active and leaving the house to take part in community activities is integral to living a full life. And there are safe ways to do so if you are at risk for a fall.
We know that a fall can prove to be a game-changer for otherwise active older adults. However, older adults can take proactive steps to prevent falls.
This week, we offer some ideas for staying active and walking safely. Our resource is the well-regarded Fall Prevention Center of Excellence.
If you are walking outdoors in your neighborhood to stay active or traveling, you can reduce your risk of falls by taking some sensible steps:
— Be aware of where and when you walk: In the evenings, walk where there is plenty of light to help you see where you are going. Carry a flashlight to light the way and, this time of year, look for fallen leaves that might be slippery.
Watch out for inevitable cracks in sidewalks, holes, and uneven sidewalk levels. Of course, be extra careful during and after rainy or snowy weather. Wet surfaces will be slippery.
You might not think of your eyesight, but make sure to wear the correct eyewear while walking. Bifocals or reading glasses make it harder to see hazards on the ground. Wearing sunglasses on bright days will reduce glare;
— Stay active and safe: When walking for exercise, consider going to well-maintained places such as the track at a local high school or, in inclement weather, the shopping mall. Find or create your own walking team; walk in pairs or groups so you can alert each other of potential hazards as well as enjoy each other’s company. Wear shoes with firm soles and low heels when exercising; and
— Travel safely: Always take your time; hurrying across streets or rushing to catch a bus or train puts you at risk of falling. When climbing outdoor steps or riding public transportation, use the available handrails and move slowly.
If traveling by car, you should use extra caution walking across parking lots and in parking garages. Be aware of curbs, car stops, and changes in elevation. When crossing the street, walk in crosswalks and use curb cuts or ramps when they are present. Stop at islands in the middle of the street when available and wait for the next walk sign.
For more good ideas to prevent falls, you can check online at www.stopfalls.org.
Community Caregivers Inc. is a not-for-profit organization that provides non-medical services including transportation and caregiver support at no charge to residents of Guilderland, Bethlehem, Altamont, New Scotland, Berne, Knox, and the city of Albany through a strong volunteer pool of dedicated individuals with a desire to assist their neighbors.
Our funding is derived in part from the Albany County Department for Aging, the New York State Office for the Aging, and the United States Administration on Aging. To find out more about our services, as well as volunteer opportunities, please visit www.communitycaregivers.org or call us at 518-456-2898.
Editor’s note: Linda Miller is the Outreach and Education coordinator for the Community Caregivers.
Location:
When we think about physical activity, we typically think about losing weight or gaining muscle, perhaps the two most obvious benefits to being active. As people age, these benefits might not seem as appealing or as necessary, especially with work feeling more strenuous than it used to.
However, even if losing weight or gaining muscle aren’t on your mind, there are still many other lesser known benefits to staying active into your later years.
The Stanford Center on Longevity reports that, in 2011, twenty-eight percent of Americans aged 75 and older were getting sufficient exercise. Broken down into smaller groups (all for Americans ages 75 and up), those with the highest income had the highest percentage of people getting sufficient exercise while those with the lowest income had the lowest percentage.
As well, the center reported that males are more likely to get sufficient exercise when compared to females and those with more than a college education have the highest percentage of people in that population exercising — almost 46 percent.
While these numbers may not seem bad, they indicate that less than half of Americans aged 75 and up are getting enough activity, while the amount of sedentary activity has increased. There is clearly room for improvement.
Whether it’s planned exercise or a physical activity that is already built into your day, staying active has many benefits for disease maintenance, mental health, and aging in place. Among other benefits, a Surgeon General’s Report mentions that physical activity can:
— Help control joint swelling and pain related to arthritis;
— Help maintain healthy bones, muscles, and joints;
— Reduce the risk of falling and fracturing bones; and
— Reduce symptoms of anxiety and depression and may improve mood and feelings of well-being.
As our loved ones age, it’s important to encourage them to get up and move around. The same advice applies to each of us!
Even if it’s only for a walk around the block when it’s cool outside or a walk around the mall if it’s too hot to be outside, there are clear benefits to staying active as we age. If you’re looking for a buddy to stay active with, many community centers and local senior centers have group exercise programs.
By joining a group and meeting some new friends, staying active can feel less like a chore and more like a hobby. Regardless of how you and your family members choose to stay active, make activity a priority to maintain mental health, to age in place, and to maintain or improve overall well-being.
Fall calendar
The first step to becoming a Community Caregivers volunteer is to attend a one-hour orientation session. Come and find out how you can help your neighbors by volunteering with us!
Most sessions are held at our Guilderland office with convenient parking: Community Caregivers Inc., 2021 Western Ave., Suite 104, Albany, NY 12203.
Registration in advance is required. Please register by calling 518-456-2898 or by email at
Here are the dates for orientation sessions:
— Thursday, Sept. 20, at noon;
— Tuesday, Oct. 2, at 1 p.m.;
— Thursday, Oct. 18, at 1 p.m.;
— Tuesday, Nov. 6, at 11 a.m.; and
— Thursday, Nov. 15, at 1 p.m.
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher, and incoming second year medical student at Albany Medical College. She was an intern with Community Caregivers during the summer and wrote articles on health and wellness, which are both topics she is passionate about.
Location:
It seems like everywhere we look we’re being encouraged to live a healthier life. From watches that track the number of steps we take each day to water bottles that are smart enough to tell us when we need to hydrate, technology is trying to improve our health however it can.
While doing some reading, I came across a difference between two terms that are often used interchangeably — physical activity and exercise. While they sound the same, they actually mean different things.
The National Institute of Health specifies that both “physical activity” and “exercise” refer to movements you do voluntarily that burn calories. However, “physical activity” can be more general activities that get you moving, while “exercise” is a specifically planned, structured and repetitive activity.
Some examples of physical activity are gardening, cleaning the house, and walking your dog, while examples of exercise include going on a brisk walk or jog or doing yoga. Both physical activity and exercise can improve your health and prevent the worsening of illnesses you may already have.
Since both kinds of movement are beneficial, why would you choose one over the other? Many people are intimidated by the word “exercise” and feel it will be too hard for them.
Perhaps you used to jog or run regularly, but since hurting your ankle you’re scared to start back up. Or maybe you played a sport when you were younger, but don’t think it’s wise to start playing it again.
If either of these cases sounds like you, or you just hate the thought of exercising, finding ways to increase your physical activity may be a good fit. Finding activities you enjoy doing or that are easy to incorporate — like gardening, walking around your house while talking to a friend on the phone, taking the stairs instead of the elevator, and playing with your grandkids at the park — can increase your physical activity.
If you are the kind of person who prefers to plan activity into your day, scheduling a time to exercise might be a better fit for you. Remember to vary the types of exercise you do to incorporate cardiovascular exercise as well as weight training and flexibility to feel your best. For those with Medicare, some Medicare Advantage Plans cover a membership at the YMCA or other facility to give you access to group fitness classes and exercise equipment.
Regardless of how you choose to keep moving, staying active is important for “aging in place” and for mental health. The Centers for Disease Control and Prevention highlight that physical activity can reduce the risk of depression and can help you sleep better at night. As well, it can help keep skills like thinking and learning sharp.
Individuals reap multiple benefits from physical fitness, ranging from an increase in physical strength and flexibility to improved mental health. These benefits extend further — by increasing the chance that older adults can continue to live independently in their own homes.
The best way to stay active is to find something you enjoy doing alone or with a friend. When staying active is doing something you love rather than doing something you see as a chore, you’re more likely to stay with it and make time to do it.
If you’re looking for more suggestions for physical activity or exercise you can incorporate into your life, search for “NIH Go4Life” in your web browser to read more.
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher, and incoming second-year medical student at Albany Medical College. She was an intern with Community Caregivers this summer and wrote articles on health and wellness, which are both topics she is passionate about.
Location:
It seems like whenever we go to the grocery store, we walk up and down the aisles unsure of what to get. From claims like “high in fiber” to “low in sugar,” how do we actually know what the healthy option is?
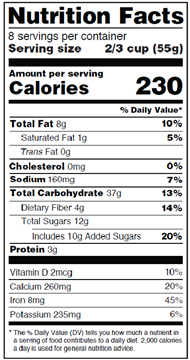
The first step to making healthier choices in the grocery store starts with knowing how to read a nutrition label. Even if you already feel like you’re a pro at reading nutrition labels, it’s worth knowing what the new nutrition labels will look like. Here is a mockup of a label from the federal Food and Drug Administration’s website.
When looking at a nutrition label, our gaze typically goes straight to calories. However, before we even get there, it’s helpful to start with “Serving size” and “Servings per container.”
Serving size reflects the portion of food that the label is for and can be very misleading. Even foods that look like they’re only one serving can easily be two or three. For example, a frozen dinner might be two servings or a muffin might be three to four servings, even if you’re planning to eat the entire thing in one sitting.
Serving size is important when you start scanning down the rest of the label, especially calories, fat, sodium, fiber, and sugar. Moving down the label, your eyes will land on “Calories” next.
While there’s no good or bad number of calories, be aware that the calories are for a single serving. In the example with the frozen dinner — there may be 220 calories per serving with two servings, which means that the whole meal has a total of 440 calories.
Moving down the label, you will come to “Total Fat.” More important than total fat is “Saturated Fat.” This is the unhealthy kind of fat that comes from solid fats like butter, lard, cheese, and vegetable shortening and should be limited in your diet.
Dietary guidelines suggest that normal, healthy adults should consume no more than 10 percent of their daily calories from saturated fat. If you’re eating 2,000 calories a day, that’s about 200 calories from saturated fat or about 20 grams of saturated fat a day.
However, the less saturated fat you consume the better — focus instead on unsaturated fats from nuts, seeds, and oils. And remember, this number is per serving as well.
Next up is “Sodium,” commonly referred to as salt. While the dietary guidelines suggest consuming less than 2,000 milligrams of sodium a day, publications from Harvard Health state that the average American consumes 3,400 milligrams of salt — nearly twice as much as the recommended amount!
According to the federal Centers for Disease Control and Prevention, much of this sodium comes from canned foods like pasta sauce and soup; cold cuts; and, surprisingly, bread. High intake of sodium has been linked to high blood pressure and is certainly a nutrient to look out for on nutrition labels.
Skipping past carbohydrates, see if your nutrition label has anything listed next to “Fiber.” Fiber is found in fruits, vegetables, and whole grains, and is important for bowel regularity and helping you feel full after meals.
While the dietary guidelines suggest men should consume 38 grams of fiber and women should consume 25 grams of fiber daily, the most recent National Health and Nutrition Examination Survey found that Americans are not meeting these goals.
This survey found that most American adults are only meeting 50 to 60 percent of their fiber goal and only 8 percent of Americans meet the recommended amount of fiber intake daily. These numbers make fiber a major nutrient of concern. Look for foods that are high in fiber by choosing fresh fruits and vegetables, bread made with 100-percent whole-wheat flour, whole-wheat pasta, and brown rice.
Finally, the last place to look is “Total Sugar.” In an updated nutrition facts panel, there will be a subcategory for “Added Sugar,” which is really what you want to pay attention to. The Dietary Guidelines recommend the same percentage for added sugar as they do for saturated fat — no more than 10 percent of your total calories should come from added sugar.
Again, if you’re eating 2,000 calories per day, this is about 200 calories from added sugar or about 50 grams per day. If this seems like a lot, it’s because it is!
While the guidelines allow for more added sugar than we necessarily need, it’s important to note that both the United States Department of Agriculture and the World Health Organization recommend only 22 to 25 grams of added sugar per day, or about 5 percent of total calories from added sugar.
Since added sugar has been linked to weight gain, obesity, and Type II diabetes, the less you consume, the better. You’re not missing any nutrients if you try to avoid it.
Finally, we’ve arrived at “Protein” at the bottom of the label. While protein helps us feel full and satiated, many people incorrectly think the more protein we eat, the better.
The actual guidelines for protein consumption are 0.8 grams per kilogram of body weight because too much protein can tax your kidneys. To calculate how much protein you need daily, divide your body weight in pounds by 2.2 (this gives you kilograms) and multiply that number by 0.8. For example, I weigh 130 pounds. Divided by 2.2, that’s roughly 59 kilograms. Multiplied by 0.8, I only need 47 grams of protein daily.
That’s the equivalent of one Greek yogurt and half of a chicken breast. Even with eating a vegetarian or vegan meal for one or even two of my meals daily, I can still get more than enough protein without overloading my kidneys.
Grocery-store aisles can be a confusing place. Knowing what nutrients to look for, remembering to take note of the number of servings per container first, and starting from the top and working down is a good strategy to help make healthier choices with so many food options out there.
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher, and incoming second-year medical student at Albany Medical College. She is interning with Community Caregivers this summer and is writing articles on health and wellness, which are both topics she is passionate about.
Location:
In my last column, I wrote about how calorie needs change with aging and a decrease in appetite caused by many factors is part of the aging process. While there are medications to increase or decrease appetite approved for physician prescription, there are other variables you can adjust at home to change your calorie intake.
The Delbouef Illusion is a visual perception bias that indicates how the size of plates and color contrast between a plate and food can impact serving sizes. In fact, much research has shown that the size of your plate and color contrast between your plate and your food can have a significant impact on portion size.
Dr. Brian Wansink, Ph.D., of Cornell University’s Food and Brand Lab, looks at the psychology behind eating behavior. Working with other researchers, he looks at different factors that play into our eating habits.
To test the Delbouef Illusion, the Food and Brand Lab conducted an experiment in which, among other things, some participants served themselves on smaller dinnerware while others served themselves on larger dinnerware. As well, some participants served themselves food on a plate that was a similar color to the food (pasta with red spaghetti sauce on a red plate) and others served themselves using a plate that was a contrasting color from the food being served (pasta with red spaghetti sauce on a white plate).
The study found that people serve themselves more food when using large dinnerware and dinnerware that is a similar color to the food they’re eating. However, people serve themselves less food when using smaller dinnerware and when their food is a contrasting color to their dinnerware.
As appetite decreases with age, these are tools that you, as a family caregiver, can use with your loved ones to increase their calorie intake. While it can be frustrating to argue with loved ones about eating, using plate size and color contrast is an easy way to “trick” them into increasing or decreasing their calorie intake.
If you’re looking to encourage your loved one to eat more, try having them serve their food on a larger plate or using a plate that is a similar color to the food you’re eating. If you’re trying to decrease calories, try using a smaller plate or a color that will pop against the food you’re having at that meal.
Food doesn’t always have to be a fight. Since lots of what we eat is behavioral, sometimes it’s easier to adjust our behaviors to meet our goals instead of choosing different foods. If you’re interested in reading more about food behaviors, search online for “Food and Brand Lab” to read more and see how you can make small changes for a large impact.
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher and incoming second-year medical student at Albany Medical College. She is interning with Community Caregivers this summer and will be writing articles on health and wellness, which are both topics she is passionate about.
Location:
It seems as though every year we get older, it gets easier to gain weight — to a point. For most of our adult lives, a decrease in physical activity and decrease in muscle mass make it easier to pack on pounds. Due to these factors, calorie needs decrease even though some vitamin and mineral needs increase.
However, as we age past our older adult years, our appetite tends to drop due to a variety of factors. For that reason, we need to encourage the older people in our lives to eat more calorie-dense foods or eat small meals more often.
All this can be a bit confusing. When do calorie needs decrease and when does appetite drop? Why do all of these changes happen? What signs should I be looking out for?
To start, calorie needs are determined based on height, weight, gender, and age. From there, calorie needs may increase based on what you spend most of your day doing and the amount of physical activity you’re participating in.
There a few equations that calculate this information including the most popular — the Harris Benedict equation. If you’re interested in calculating the numbers for yourself, a quick search on Google for “Harris Benedict equation” can provide you with an easy-to-use calculator if you know your height and weight.
As you get older, your muscle mass begins to decrease even if you don’t notice it, a condition called sarcopenia. Muscle that breaks down is replaced with fat and fibrotic scar tissue, neither of which have the same strength capabilities as muscle. Since muscle burns more calories than scar tissue and fat, our calorie needs decrease as well.
Aging also brings changes in taste, a dry mouth (a condition known as xerostomia), dental problems, and neurological conditions that can decrease appetite and interest in eating. While this may seem like a good thing given the decrease in calorie needs, it can actually cause additional health complications such as significant weight loss and malnutrition if unnoticed or untreated.
Significant weight loss, defined as a weight loss of 5 percent in one month, 7.5 percent in three months, or 10 percent in six months, can cause the loss of fat that protects our internal organs such as the kidney. This can cause infection or problems with urination and may require a surgical intervention.
Malnutrition, which is a problem with the balance of nutrients, can cause a loss of muscle, increase in frailty or fracture risk, and increased risk of pressure ulcers if a person has limited mobility.
Recognizing the early symptoms of severely decreased appetite can be difficult. Pay attention to changed eating habits or if a person is skipping meal times more often. If you do notice something or a person is frequently declining to eat because they’re just not hungry, there are a few things you can do:
— Encourage small, frequent meals;
— Focus on calorie- and nutrient-dense foods such as nuts or nut butters, avocados, and whole fat yogurt;
— Speak with your doctor about adding nutritional shakes such as Ensure or Boost to your loved one’s diet.
While calorie needs may decrease throughout our life, not consuming enough calories can pose an even bigger risk. Paying attention to your loved one’s eating habits is as important as making sure they take their medications every day.
If you’re concerned, ask your loved one if there are specific reasons why he or she may not be eating as much and voice concerns about food intake at his or her next doctor’s visit.
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher and incoming second-year medical student at Albany Medical College. She is interning with Community Caregivers this summer and will be writing articles on health and wellness, which are both topics she is passionate about.
Location:
Have you noticed someone you love adding salt to their food more often? Or perhaps adding sugar to coffee they used to always take with only cream?
Dysgeusia, altered taste sensation, and hypogeusia, decreased taste sensation, are both common conditions in older adults. However, even though scientists and the National Institute of Health estimate that up to 15 percent of adults suffer from conditions related to decreased or altered taste or smell, many people are unaware that they are experiencing any symptoms.
The cause of dysgeusia and hypogeusia can be varied according to “The Impact of Aging and Medical Status on Dysgeusia,” an article published in The American Journal of Medicine in July 2016. Many medications may cause these conditions as a direct side effect or may cause decreased saliva production (a condition called xerostomia), which can cause them as well.
As our loved ones get older, the list of medications they take tends to get longer, which is one reason why older people are at a greater risk for having these conditions.
Alternatively, the normal anatomy of the nose and mouth can be the culprit. While the tongue has three nerves that run from parts of the tongue to the brain, acting like a safety net in case one is damaged, the nose has only one set of nerves that run directly to the brain.
Since the brain slows down and ages like the rest of the body, older people are more at risk for these conditions. People with dementia, Parkinson’s, or Alzheimer’s are at even higher risk.
Due to decreased or altered taste, many older people may add extra salt or sugar to their food to help it taste better or choose foods higher in salt and sugar. While this may not seem like a problem initially, excess sodium can raise blood pressure and added sugar can contribute to weight gain or high blood sugar. If your loved one is already suffering from conditions such as hypertension or diabetes, this could be an especially big problem.
Additionally, added sugar can cause cavities, which have been linked to diabetes, heart disease, and kidney disease.
On the other side of excess intake is inadequate intake or anorexia. People suffering from dysgeusia and hypogeusia may stop eating, claiming the food tastes “off.” This is seen especially in intake of proteins like red meat, fish, and seafood, which many people with hypogeusia and dysgeusia find unappetizing. While too much sugar and salt are a problem, anorexia can lead to malnutrition, wasting and numerous other health problems.
Clearly, it is important to recognize the symptoms of dysgeusia and hypogeusia in order to treat them and make dietary adjustments early on. Some tips and alternate strategies for reducing the risks linked to these diseases are:
— Educate your loved one and learn how to make adjustments to food together;
— Address the underlying issue: Is the problem due to medication? Can the medications they are on be adjusted to reduce these side effects?
— Encourage your loved one to improve flavor in foods by adding fresh herbs and spices instead of salt;
— Suggest the use of alternative sweeteners such as Stevia and Splenda instead of sugar to keep calories and blood sugar down and reduce the risk of cavities; and
— Encourage consumption of cold foods as they’re less likely to trigger odors that may be off-putting.
Slow changes over time and encouraging healthier strategies can help keep us and our loved ones healthy for many more years. As always, if there is any concern about you or your loved one suffering from these conditions, call your doctor to discuss treatment options. Managing these conditions can improve quality of life and reduce risk of other chronic illnesses. For more information, consult the National Institute of Health online about taste disorders at: goo.gl/Ybjkee.
****
Editor’s note: Sarah Roger is a Registered Dietitian Nutritionist, 200-hour Registered Yoga Teacher, and incoming second-year medical student at Albany Medical College. She is interning with Community Caregivers this summer and will be writing articles on health and wellness, which are both topics she is passionate about.